Could understanding the history of anti-vaccine sentiment help us to overcome it?

Sarah and her brother Benjamin (not their real names) have never seen eye to eye. She’s a professional scientist, he – according to Sarah’s description – is someone who is susceptible to conspiracy theories. They maintained an uneasy truce until a few weeks ago. Tensions came to a head when Sarah was on the phone to her mum, talking her through the online procedure to book a slot for her Covid-19 vaccination.
If she was still having trouble after they rang off, Sarah suggested, she could ask Benjamin to come over and help. Mother and son live close by and a long way from Sarah; they’ve shared a bubble this past year. “There was a silence,” Sarah says. “And then she replied that he didn’t want to. He’s against the vaccine. Well, that was it for me. You can’t help your 77-year-old mum do something that might save her life? I’m sorry, that’s wrong.”
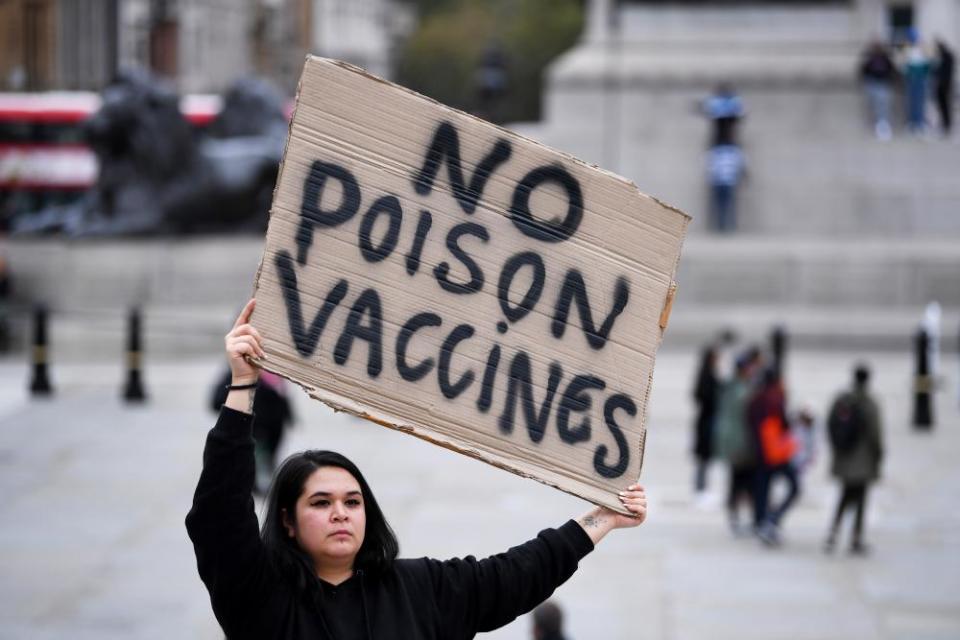
This happened in France, where surveys tell us levels of vaccine hesitancy are particularly high, but similar confrontations are taking place in many countries. Now tensions are coming to a head because the long-awaited vaccines are finally being administered and talk is having to be translated into action – or not. There’s a lot riding on the outcome. Statisticians estimate that close to 90% of us will need to get vaccinated in order to achieve herd immunity.
Experts refer to vaccine “hesitancy” because it covers a spectrum, from those with very narrow and specific doubts – or sometimes just questions – to the extreme and unassailable anti-vaxxer, and understanding that is key to thinking about how hesitancy shapes people’s behaviour. One optimistic school of thought holds that much hesitancy will just melt away. In August, Paul Offit, the head of the Vaccine Education Center at the Children’s Hospital of Philadelphia, warned against taking surveys that were then showing worryingly low levels of willingness to get vaccinated too seriously, because no vaccine existed, and, in a data vacuum, it was reasonable for people to be sceptical. And indeed, a recent survey showed that the proportion of French people willing to get vaccinated jumped from 39% in December to 51% in January – a pattern repeated in other countries.
But others see a different trend unfolding. “The pandemic has increased empathy for people who are hesitant,” says Bernice Hausman, a cultural theorist at Penn State University and the author Anti/Vax. Partly it has done so, she believes, by highlighting structural inequalities in healthcare and their historical roots. Lately, for example, US media have been full of talk of the infamous Tuskegee study of the middle 20th Century, which unethically tracked the course of syphilis in African-American sharecroppers without ever offering them treatments known to be effective. Public perceptions have undergone a huge shift during the Covid pandemic, Hausman says, from seeing the vaccine-hesitant as victims of misinformation, to seeing them as mistrustful for valid social and historical reasons.
It’s too early to say how these opposing forces will shape vaccine uptake. “I think right now we’re in a bit of a honeymoon period,” says the anthropologist Heidi Larson, who directs the Vaccine Confidence Project at the London School of Hygiene & Tropical Medicine. Vaccine is scarce and supplies are being reserved for the most vulnerable, who tend to be enthusiastic. “We may be looking at a bumpier road in February and March, when it moves into the broader population,” she says.
Could history shed light on what to expect, and how to steer it for humanity’s collective benefit? Paula Larsson, a historian of medicine at the University of Oxford who studies anti-vaccination movements, thinks it can. Hesitancy is as old as vaccines, she says. For at least a century after Edward Jenner came up with the first vaccine in 1796, against smallpox, vaccination was a much riskier enterprise than it is today, though the protection it conferred still far outweighed any harms it provoked. It wasn’t always carried out in the most sanitary conditions, which meant it sometimes caused secondary infections. The side-effects could be unpleasant and lingering, and, if they forced a worker to take time off work, could result in a loss of income.
These were legitimate concerns throughout the 19th century, when the smallpox vaccine was the only one most people were offered, and they resurfaced during epidemics when health authorities made efforts to increase vaccine coverage. What also surfaced in epidemics were individuals Larsson refers to as “white knights”, who harnessed popular concerns to drive their own agenda and paint themselves as heroes.
She gives the example of Dr Alexander Ross, the author of a pamphlet that circulated widely in Montreal in 1885, during an outbreak of smallpox in the city. “Talk no longer of Russian tyranny,” railed Ross, implying that the Russians – just then persecuting Jews in pogroms – had nothing on the city health officials when it came to trampling civil liberties. He assured his readers that vaccination did not prevent smallpox, but that it did cause other nasty diseases such as syphilis and smallpox itself, and it killed children “outright”. What’s more, he claimed, there wasn’t really an epidemic in the city and, if there was, the best way to protect yourself was “pure air, cleanliness and temperance”. For “proof” he offered the testimonies of a number of individuals whose names were prefixed by “Prof”, “Dr” or “Sir”.
Ross’s tactics have been the tactics of the figureheads of anti-vaccination movements throughout history, Larsson says: talk down the disease threat (smallpox killed one in three of those it infected and left most of the survivors scarred for life), talk up the vaccine threat, hint at a bigger conspiracy and appeal to other authority figures who, like you, dare to challenge the consensus. Because of their use of disinformation, she reserves the pejorative label “anti-vaxx” for these individuals and makes a clear distinction between them and the majority of the vaccine-hesitant (Ross, it turns out, got himself vaccinated during the epidemic).
The most obvious recent reincarnation of Ross is Andrew Wakefield, the disgraced former doctor whose fraudulent 1998 study reported an association between the measles, mumps and rubella (MMR) vaccine and autism, but others have emerged since the beginning of this pandemic. One is Judy Mikovits, the virologist whose debunked claims featured in a widely viewed pair of conspiracy theory videos entitled Plandemic even before a Covid-19 vaccine existed. Now that several such vaccines have been approved in a limited way, Larsson expects other white knights to step up. “We will probably see a lot of these people in the next year,” she says.
History also teaches us that the reasons people are hesitant about vaccines are diverse, complex and exquisitely sensitive to social and political context. During the Montreal outbreak, for example, resistance was fuelled by pre-existing tensions between the city’s francophone and anglophone populations. “French-speaking workers resented the upper-class English doctors who wanted to stick needles into them,” Larsson says. It didn’t help that a contaminated batch of vaccine caused some cases of the skin infection erysipelas early on. And yet it was only later, when the authorities made vaccination compulsory, that resistance erupted into riots.
Historically, mandates often crystallised anti-vaccine sentiment, in part because of fears that they would be applied in a brutal or discriminatory fashion. Such fears were not unfounded. There are grisly accounts of ethnic minorities being vaccinated at gunpoint, or medically vulnerable populations being forcibly given experimental concoctions. Delivering the 1905 supreme court ruling known as Jacobson v Massachusetts, which upheld US states’ right to mandate vaccination, the civil war veteran Justice John Marshall Harlan implicitly acknowledged the brutality of the mandate when he stated that collective self-defence may sometimes involve risk of bodily harm to the individual, as when a citizen was compelled “to take his place in the ranks of the army of his country and risk the chance of being shot down in its defence”. Vaccine sceptics were a step ahead of him. At that time, the term “conscientious objector” referred to someone who objected to vaccines; it was only during the first world war that it came to mean a person who objected to taking up arms. But the 1905 ruling galvanised them, and in 1908 the Anti-Vaccination League of America was created. “Vaccination has always been violent,” says Hausman.

The number of diseases for which vaccines existed began to increase rapidly at around the turn of the 20th century, but progress came with setbacks. In 1929, in Lübeck, Germany, a contaminated batch of the BCG vaccine for tuberculosis led to the deaths of 72 babies and a resurgence of anti-vaccine sentiment. Yet such accidents, or scandals, drove improvements in oversight, to the point where Offit could write in 2006 that vaccines enjoyed a safety record “unmatched by any other medical product”. And they transformed human health. Smallpox killed more than 300 million people in the 20th century before claiming its last victim in 1978. Yet despite vaccines’ impressive track record and far more sophisticated approaches to mandates – involving fines rather than guns, for example, and allowing exemptions on religious and other grounds – vaccine hesitancy is at a 20-year high, according to some polls, and growing.
Efforts to educate people haven’t worked, Hausman says, and a clue as to why lies in the shift that has happened this year – from understanding hesitancy as an information issue to understanding it as one of trust. Public health experts focus on the benefits of vaccination to populations, she says, “but people don’t experience vaccine injury at the population level, they experience it personally”. It’s therefore important to understand their concerns, because a person of African American heritage, say, may have very different ones from a person with allergies who is reading about the – few, it must be emphasised – cases of anaphylactic shock that have been reported in recipients of some Covid-19 vaccines.
In her recent book, Stuck, Heidi Larson quotes, and agrees with, the Australian epidemiologist Stephen Leeder: “Facts are not rejected because they are seen as being wrong, but because they are seen as being irrelevant.” Vaccine educators are on to this, and increasingly privilege stories over statistics. Someone you know had a bad reaction? OK, let me tell you about a couple last week, your age, who got the vaccine and are doing fine. They also realise that different kinds of people should be saying these things. As the marketing expert Stacy Wood told Science recently, it shouldn’t always be Anthony Fauci, as effective a spokesperson as he is.
The storytelling approach has its critics. The Spectator recently dismissed it as showing “a supercilious contempt for ordinary people”. But it’s exactly the approach that has been used so successfully by true anti-vaxxers, who have harnessed social media and who, according to a recent report published by the international non-profit the Center for Countering Digital Hate, are now coordinating their efforts to try to drive long-term vaccine hesitancy. Plus, says Hausman, it isn’t just “ordinary people” who are more influenced by stories than stats; powerful ones are too, including some of those taking decisions in this pandemic.
It’s easier to stop people from taking an action than to persuade them to take it, which means that Team Jenner will always have to work harder than the opposition. “All the white knights have to do is sow a doubt,” says Larsson. But the main lesson from history is that it’s not just what they do that matters. Underpinning the success of vaccination is a strong social contract, and ours is fraying. As the author of Stuck writes: “Immunisation has become a profound test of our ability to cooperate.”
Laura Spinney is the author of Pale Rider: The Spanish Flu of 1918 and How It Changed the World

 Yahoo Finance
Yahoo Finance 